Hospital management isn’t just about handling emergencies after they happen. It’s about planning ahead, spotting potential problems early, and making decisions that prevent issues before they arise. Resource allocation in healthcare has always been a complex task, but now, with predictive analytics, hospital leaders have the tools to optimise resources in real time.
In a recent report, 92 percent of healthcare leaders in Singapore reported already adopting or planning to adopt predictive analytics, leading globally.
This shift is happening across the world, with China at 79 percent, and Brazil and the U.S. at 66 percent, all moving towards smarter, more efficient resource management. This growing adoption of predictive analytics is changing the way hospitals approach resource management.
But what is resource allocation in healthcare in practice?
It’s not just about managing beds or staffing; it’s about understanding the interdependencies across departments and predicting needs before they arise. Let’s explore what is resource allocation in healthcare. And what it truly means inside a modern hospital system.
Is Your Hospital Built To Think Ahead Or Stuck Reacting Too Late?
Resource allocation in healthcare is no longer about fixing problems after they happen. It’s about preventing them before they begin. That’s where predictive analytics in hospital resource allocation becomes a game changer. This isn’t just a capacity issue. It’s a planning issue.
Hospitals using AI are already seeing the difference. They are predicting surges, preparing staffing early, and reducing wait times. They’re not reacting. They’re staying ahead.
Now is the time to ask the tough question. Is your hospital operating with real foresight? Or still, relying on last-minute decisions?
Let’s say your ED is full by noon every day. The patients keep coming, but beds are tight. What if you had a model that told you at 8 a.m. what was coming? What if your ORs adjusted cases or your discharge teams sped up just two discharges before noon?
This is not the future. This is already working in leading hospitals around the world.
Hospital resource optimisation using predictive analytics is not a one-time project. It’s a shift in how hospitals plan, think, and lead.
If your team wants fewer delays, safer care, and stronger performance, predictive planning must be part of the core system.
It’s time to stop reacting. And start preparing.
What Resource Allocation in Healthcare Really Looks Like in Modern Hospitals
Most people think resource allocation in healthcare is only about managing beds or scheduling nurses. But inside a hospital, the reality is much more complex. One delay in one department can cascade across the entire hospital system.
Take this for example. When a patient’s discharge is delayed by just a few hours, the next admission can’t move in. That holds up the emergency department. Then, the waiting area gets crowded, staff get overwhelmed, and surgical cases may get postponed. This is not just about availability; it’s about timing and coordination. Predictive Analytics in Telemedicine can support smarter scheduling and faster decision-making to help prevent such delays.
In another case, when an operating room runs behind schedule, the post-anesthesia care unit (PACU) gets full. ICU beds that should be freed up remain occupied. As a result, new critical patients wait longer than they should. This delay isn’t caused by a lack of infrastructure. It’s a breakdown in flow.
This is why hospital resource optimisation using predictive analytics matters more than ever. Modern hospital systems are deeply connected. One unit’s delay becomes another’s problem in minutes.
Understanding what is resource allocation in healthcare means seeing the hospital as a living system. Every staff shift, every equipment use, and every patient transfer is part of that system. Predictive tools give leaders the ability to look ahead. Instead of reacting to problems, they can prepare for them.
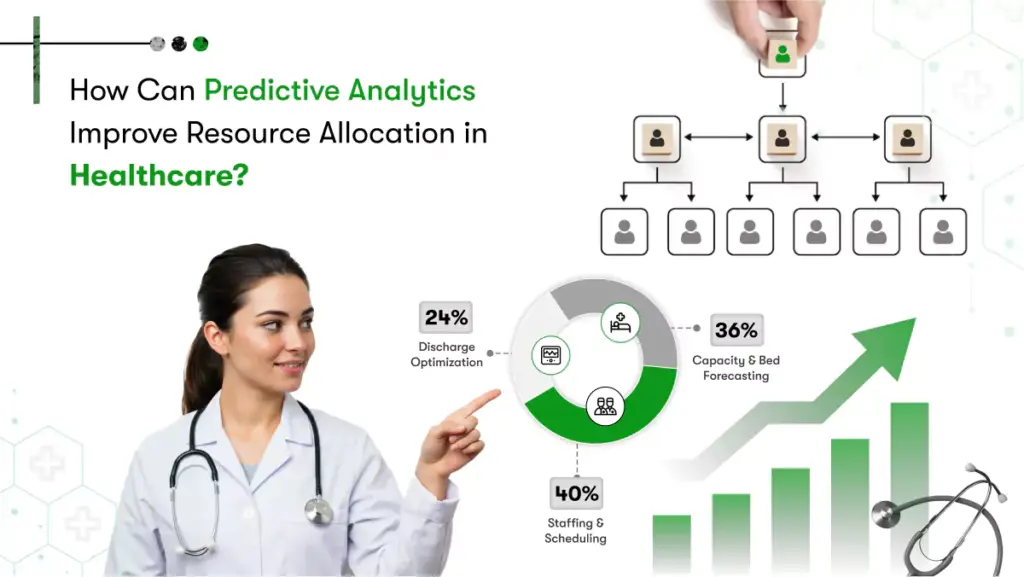
Predictive analytics in healthcare for resource allocation allows hospitals to forecast patient volume, prevent bottlenecks, and align staff and space before the crisis hits. In short, it’s not just about managing what you have. It’s about knowing what’s coming next. This is the future of AI for hospital resource planning.
Let’s take a closer look at how predictive tools connect all the dots of fragmented data to make informed decisions.
How Predictive Analytics For Better Resource Allocation In Healthcare Turns Fragmented Data Into Future-Ready Decisions
Hospitals run on data, but most of it stays scattered. Bed availability is tracked in one system. Staffing is managed in another. Supply use is recorded elsewhere. Often, these systems don’t talk to each other. That’s one of the biggest challenges in resource allocation in healthcare today.
Healthcare predictive analytics consulting for resource allocation helps fix this. It connects the dots between EHRs, bed tracking tools, staff schedules, ADT feeds, transport logs, and even supply chain systems. Instead of seeing parts, you get a complete picture of what’s happening and what’s about to happen.
In traditional settings, you look at yesterday’s reports to plan today. But predictive tools change that. They turn static data into live projections. You don’t just see how many beds are full. You see which ones will open soon, where bottlenecks will likely form, and how many patients are expected by shift change.
This shift matters. It moves you from reacting to anticipating from broad KPIs to unit-level actions. This is the core of hospital resource optimisation using predictive analytics.
Take Cleveland Clinic, for example. Their AI-powered command centre pulls live data across departments. It predicts staff shortages, OR backlogs, and ICU congestion before it happens. That’s not just planning. That’s foresight in action. With AI for hospital resource planning, you gain time, clarity, and control when it matters most.
Why Top-Performing Hospitals Are Abandoning Reactive Resource Allocation in Healthcare
In a busy hospital, minutes matter. But traditional systems often make leaders wait hours for updates. Bed tracking is manual. Staffing decisions are based on static spreadsheets. Operating room schedules are managed on fixed timelines, even when patient flow changes.
This kind of planning worked when hospitals had predictability. But today, demand shifts very swiftly. Delays in one area can affect other departments too. That’s why resource allocation in healthcare can no longer rely on guesswork or outdated data.
The real issue isn’t just availability. It’s timing and coordination. By the time you realise there’s a shortage, it’s already too late.
This is where predictive analytics to optimise hospital resource allocation makes a difference. It helps hospitals move from reacting to planning ahead. Predictive tools use real-time data to show what’s likely to happen in the next few hours or days. This helps leaders adjust staffing shift schedules or reschedule surgeries before the problem hits.
One of the examples of resource allocation in healthcare is HonorHealth in Arizona. They partnered with Qventus to use AI that predicts patient discharge times. The system sends alerts to staff and care teams so they can act early. As a result, patient flow improved, and the hospital freed up beds faster.
This is AI for hospital resource planning in action. Hospitals that use it are not waiting for reports. They’re making decisions based on what’s coming next. And that’s the shift from reactive to proactive care.
What’s Actually Working In Predictive Resource Allocation In Healthcare Today
Around the world, hospitals are seeing real results from predictive systems. These tools don’t just show what’s happening. They help prevent what could go wrong.
One of the best examples of resource allocation in healthcare is OR load balancing. At Cleveland Clinic, predictive tools track how delays in surgery can affect PACU and ICU availability. The system gives live suggestions on how to reassign slots or flag overloads before they happen. This keeps patients moving, and staff focused.
Another example is ICU surge prediction. Many hospitals now use AI models to forecast bed demand based on ED trends, admissions, and discharge rates. The U.S. Froedtert Health built predictive models that helped them prepare ICU beds in advance. This allowed smoother admissions and avoided chaos during peak hours.
he U.S. Froedtert Health’s predictive model also showed real-time discharge forecasting. Hospitals using tools like Qventus or GE’s digital twins can predict when patients are likely to leave. This helps staff plan better, reduce wait times, and admit new patients faster. That’s smart hospital resource optimisation using predictive analytics.
These aren’t future ideas. They are working today.
The factors affecting resource allocation in healthcare, like unexpected patient surges, staff availability, and procedure timing, are now being managed better by prediction, not reaction. That’s the real win.
How Hospitals Predict Capacity Needs To Improve Resource Allocation in Healthcare Before A Crisis Even Begins
Hospitals rarely get time to prepare. Admissions can spike without warning. A few delays can throw off an entire shift. That’s why real-time planning is no longer optional. It’s necessary.
Modern systems now use live data to stay ahead. Predictive analytics in hospital resource allocation brings together inputs from EHRs, ADT logs, staff schedules, and even IoT sensors. This data helps hospitals see problems before they happen.
For example, Froedtert Health in Wisconsin built AI predictive models for personalized healthcare treatment that monitored patients’ conditions and, thereby, patients’ flow in real-time. These models track admissions, discharges, and transfers to forecast ICU demand. With these early signals, the hospital can free up staff and beds hours before the surge hits.
Let’s consider a hospital in Dubai. Its emergency department sees a rise in high-acuity patients. The AI dashboard, trained on historical spikes, predicts a 20 per cent increase in ICU admissions within the next six hours. Based on this, the hospital reschedules one elective surgery, reroutes a new admission to another ward, and assigns two extra ICU nurses. Instead of last-minute panic, the staff is prepared well in advance.
That’s the power of AI for hospital resource planning. It transforms hospitals from reactive responders to prepared systems. When data flows in continuously, planning becomes smarter, faster, and safer.
Which Predictive Models Are Shaping Future-Ready Hospital Operations Using Resource Allocation in Healthcare
Not all AI is built the same. Hospitals today are moving beyond basic reporting tools. They’re using smart models that understand patterns, relationships, and impact.
One major example is the digital twin. GE Healthcare now offers hospitals a real-time simulation of their own systems. Leaders can test “what if” scenarios like adding ICU beds or changing operating rooms times before making changes. This reduces guesswork and improves outcomes.
Another powerful tool is graph-based machine learning. These models map how patients move between departments. They show how delays in one area, like radiology, may impact surgery prep, PACU turnover, or discharge. That kind of insight helps tighten up the flow and avoid costly slowdowns in resource allocation in healthcare.
Hospitals are also using federated learning to train predictive models without sharing sensitive patient data. And in some advanced settings, reinforcement learning is helping systems make better real-time decisions by learning from past actions.
Suppose a university hospital in Singapore builds a digital twin for its emergency and surgical units. The system simulates thousands of patient flow patterns and learns that shifting radiology staffing by just 30 minutes improves scan access. This small change leads to faster surgical prep, quicker PACU turnaround, and earlier discharges. Over weeks, the system keeps learning and improving, leading to smoother operations hospital-wide.
These models are not just advanced. They are practical. They help solve the real factors affecting resource allocation in healthcare with speed, clarity, and accuracy.
Why Predictive Systems Need Transparency in Healthcare
In hospitals, decisions happen fast. When a predictive system suggests something, like reassigning a bed or delaying a surgery, doctors and nurses want to know why. Blind recommendations do not work in high-stakes environments.
That’s why explainable AI is so important. It doesn’t just give an answer. It shows the reasoning behind it.
When hospitals apply predictive analytics in hospital resource allocation, clinicians need to stay in control. The technology should support, not replace, clinical judgment.
At NHS Kettering General Hospital, an AI tool was tested for bed allocation. Instead of pushing decisions, the system explained why certain patients were better matched with specific beds. Nurses could see expected discharge times, infection control factors, and unit pressure. Because they understood the logic, they trusted the tool and used it.
At HonorHealth, the Qventus platform forecasted patient discharges and also explained the contributing factors. This gave care teams time to act and improved confidence in daily planning.
Let’s consider a private hospital in South Africa. They deploy a predictive staffing model that recommends increasing ICU coverage during late shifts. The AI points to rising ED admissions and past patterns of delayed intubation cases between 10 p.m. and 2 a.m. Because the reasoning is visible, the nurse lead agrees. The ICU is fully staffed when the patients arrive.
This is how hospital resource optimisation using predictive analytics succeeds. Trust builds when clinical teams understand the why behind each recommendation. And trust leads to better adoption and better outcomes.
How Predictive Analytics Transforms Real-world Hospital Operations Globally
Hospitals around the world are already using predictive systems to manage everyday complexity. The impact is visible and measurable.
Cleveland Clinic built a Virtual Command Center using Palantir. It tracks real-time patient flow, OR availability, staffing gaps, and ICU capacity. The system alerts teams before pressure builds up. As a result, the clinic reports better coordination and smoother transitions between departments.
HonorHealth partnered with Qventus to predict discharge times across its hospitals. The platform sends early signals to care teams. This helps prepare for new admissions, avoid ED crowding, and reduce waiting times.
In the UK, NHS Kettering piloted an AI tool to improve bed assignments. Instead of automating decisions, the system suggested placement options and explained each one. This helped nurses assign beds faster with fewer transfers.
GE Healthcare introduced digital twin models for hospitals. These simulations mirror the real operations of a hospital. Leaders can test small changes, like shift timing or bed policy, and see how they affect overall flow before making a move.
Suppose a regional hospital in Canada uses predictive analytics not only for early disease detection but also to simulate operating room (OR) capacity across two campuses. The system recommends shifting three non-urgent surgeries to the quieter site, helping prevent ICU congestion at the main campus and reducing post-operative stays. By following these insights, care teams maintain stable operations throughout the week.
These are not experiments. They are active systems shaping smarter resource allocation in healthcare.
This is how predictive analytics in hospital resource allocation creates real change. It gives hospitals the power to act early, avoid chaos, and deliver safer care at scale.
Want to know how data-driven decisions are saving hospitals money and improving patient care? Discover the ROI of Predictive Analytics in our latest blog, packed with real-world insights for healthcare providers and insurers.
How To Implement Predictive Analytics For Resource Allocation in Healthcare Step-By-Step
Implementing predictive analytics for resource allocation in healthcare may sound difficult, but with the right structure, hospitals can see results in just a few months. let’s walk through a practical example. Consider an example of a mid-sized hospital planning to decrease the emergency department boarding and improve the ICU beds availability.
Step 1: Identify The High-Pressure Areas
The hospital started by pointing the delays that were affecting both the patient care and the operations. The Patients in the ED faced long wait times, and the elective surgeries were oftenly postponed. Now, checking the ICU admission flow is more important.
Step 2: Audit Of The Current Data Systems
The hospital data team checked all the critical sources, including EHRs, ADT logs, staff schedules, and patient flow records. The data was available, but it was fragmented. The team’s started with integrating these systems to enable the accurate and real-time predictions.
Step 3: Select The Predictive Model
To forecast the total number of ICU bed openings, the hospital implemented the time-series model. It analysed the overall historical admission patterns of patients, overall discharge rates, and the real-time occupancy trends to estimate the bed availability 6 to 12 hours in advance.
Step 4: Build or Partner for the Solution
Now, the hospital partnered with a Healthcare App Development Company that is already specialises in resource allocation in healthcare. This partner approach eased the deployment of predictive models and ensured a full regulatory compliance.
Step 5: Integrate Predictions Into Clinical Workflows
The model’s forecast outputs were embedded to a live dashboard used by the ICU and ED decision-makers. It showed the total bed availability as per the shifts, resulting in more proactive staffing and the patient transfer options.
Step 6: Pilot the System and Validate Performance
A 3-week shadow mode pilot project allowed all teams to compare forecasted data with the actual outcomes. Clinical staff reviewed alerts, offered feedback, and requested minor interface adjustments before a full launch.
Step 7: Establish Governance and Ongoing Monitoring
Now, the hospital created a governance team, that includes a clinical lead and a data analyst who meet monthly. They reviewed system accuracy, shift patterns, and staff input to keep the model updated and effective.
Step 8: Train Staff and Appoint Internal Champions
Successful resource allocation in healthcare depends on user adoption. Staff across departments were trained to read and use the forecasts. An ICU nurse manager became the designated AI champion, supporting her team and encouraging use across shifts.
Thinking about creating a secure and scalable healthcare app? Start with our trusted Healthcare Software Development guide packed with simple steps and smart tips.
What Most Decision-Makers Miss When Deploying Predictive Models At Scale?
Hospitals everywhere are investing in AI. The goal is clear. Improve resource allocation in healthcare and reduce pressure on teams. But many projects stall or fail after launch. The problem isn’t the technology. It’s what gets left out.
Hospitals around the world are turning to AI to manage resources better and ease the workload on their staff. Similarly, industries like insurance are also adopting AI for fraud prevention in insurance using predictive analytics to detect fraudulent claims before they escalate. But many projects, whether in healthcare or insurance, stall or fail after launch. The problem isn’t the technology. It’s what gets left out.
Common Pitfalls: Integration and User Trust
One big mistake is treating AI like an IT upgrade. Decision-makers often focus on the model but forget the people who need to use it. Nurses, doctors, and coordinators must be part of the process. If they don’t trust the system, they won’t act on its suggestions.
Another issue is poor integration. Predictions are sent to a dashboard that no one checks during a busy shift. Or the alert comes too late to matter. For predictive analytics in hospital resource allocation to work, the insight has to show up exactly where and when it’s needed.
Let’s consider a large hospital that uses AI to predict patient discharges. The model worked well on paper. However, it didn’t notify case managers in time to adjust care plans. Discharge delays continued, and the tool was quietly dropped. Months later, with proper workflow mapping, the hospital relaunched the tool and saw real improvements in patient flow.
Turning Predictions into Action
This shows a hard truth. Hospital resource optimisation using predictive analytics is not just about smart tools. It is about changing how decisions are made. You need clinical alignment, operational support, and clear accountability.
Without that, even the best AI cannot move the needle. However, with it, hospitals can turn prediction into action and see real gains in performance and care.
Conclusion: The Role of Predictive Analytics in Improving Healthcare Resource Allocation
Predictive analytics is now essential for hospitals that want to improve care and stay ahead. As patient numbers grow and resources stay tight, hospitals need better ways to plan. Resource allocation in healthcare can’t depend on guesswork or slow manual processes. To unlock these benefits, hospitals need more than just tools. They need a partner who understands both the technology and the complexities of healthcare operations. Kody Technolab offers Healthcare predictive analytics consulting and end-to-end solutions, combining powerful software with hands-on guidance to help hospitals move from reactive to data-driven planning.
Real examples from places like Cleveland Clinic and NHS Kettering show that predictive analytics in hospital resource allocation works when it fits into daily workflows and supports clinical decisions. Beyond just hospital operations, predictive analytics in telemedicine is also gaining traction, helping remote consultations predict patient needs and optimise virtual care. For leaders who want real results, this is the time to make AI for hospital resource planning part of everyday hospital operations. If your hospital is ready to make resource management smarter, Kody Technolab can help you build the foundation and scale with confidence.