Things you see in Sci-fi movies are becoming a reality, and nowhere is this more evident than in the transformative power of predictive analytics in healthcare. Predictive Analytics technology, a fusion of advanced algorithms and vast medical data, redefines the industry. Previously, healthcare relied heavily on reactive approaches, often addressing issues only after they arose.
Now, predictive analytics signals a proactive era where foresight guides strategies and improves patient outcomes. Analyzing historical and real-time data with predictive analytics uncovers patterns and predicts future trends. So, healthcare professionals can anticipate and mitigate health risks before they escalate.
Along with preventive patient care, Predictive Analytics in Healthcare also streamlines operational efficiency, marking a significant evolution in the sector. In this exploration, we’ll study what role predictive analytics plays in revolutionizing healthcare. And how it turns data into actionable insights for better, more informed decision-making.
What is Predictive Analytics? How does Predictive Analytics in Healthcare work?
Predictive analytics has revolutionized various industries by leveraging data to forecast future events. Its journey began with simple statistical methods and evolved into a complex field incorporating machine learning and artificial intelligence. This technology gained fame for turning vast amounts of data into meaningful predictions. In healthcare, it’s particularly important for its potential to save lives and optimize care.
How Predictive Analytics Works in Healthcare
Predictive analytics in healthcare takes raw data and transforms it into insights. Healthcare providers then leverage these insights and make informed decisions, improving patient outcomes. Let’s see how Predictive Analytics converts information into wisdom.
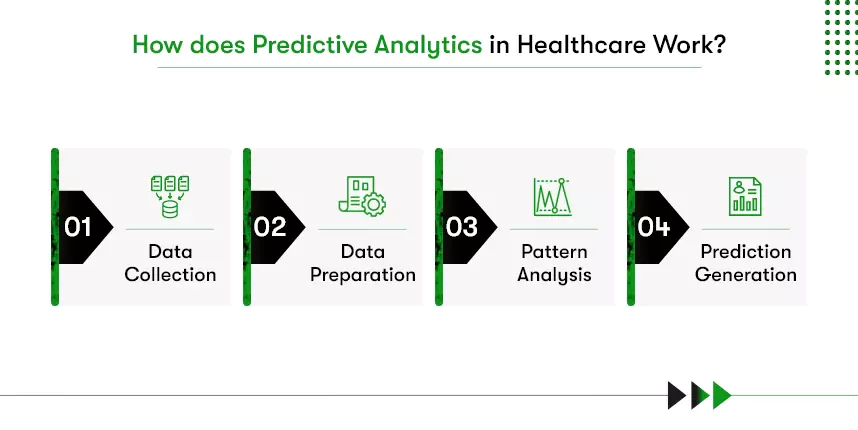
- Data Collection: The first step involves gathering extensive health-related data, such as patient medical histories, treatment records, and demographic information.
- Data Preparation: Once collected, this data undergoes rigorous cleaning and preparation, ensuring accuracy and relevance.
- Pattern Analysis: Using advanced algorithms, the prepared data is then analyzed to identify patterns and correlations crucial in understanding patient health trends.
- Prediction Generation: The final step is generating predictions about future health outcomes based on the identified patterns, anticipating health issues before they occur.
For instance, suppose there is a patient with a history of heart disease. Predictive analytics can assess their data and predict the risk of a future cardiac event. With this prediction, healthcare professionals can provide targeted care, potentially preventing the event.
Moving ahead, let us discuss the advantages of using Predictive Analytics in Healthcare organizations.
Benefits of Predictive Analytics in Healthcare
Predictive Analytics is an invaluable tool in healthcare. As a cornerstone in digital transformation in healthcare, its impact is far-reaching, paving the way for more efficient, effective, and personalized healthcare services.
Enhanced Patient Care: Since Predictive Analytics excels at predicting potential health issues before they become critical, healthcare providers intervene early, significantly improving patient health outcomes and preventing more severe complications.
Personalized Treatment Plans: By analyzing specific patient data, the technology can recommend tailored treatments, improving their effectiveness and patient satisfaction.
Optimized Resource Allocation: A key benefit is its ability to predict hospital admission rates. This foresight enables better planning and allocation of staff and resources, ensuring that hospitals are well-prepared for patient influxes, leading to smoother operations and better patient care.
Cost Efficiency: By anticipating health issues and optimizing resource allocation, predictive analytics contributes to substantial cost savings. Preventing emergency cases and better resource management also leads to a more economical healthcare system.
Proactive Public Health Management: Predictive analytics is invaluable in public health. It can identify potential disease outbreaks, allowing healthcare authorities to prepare and respond proactively, mitigating the impact on communities.
Data-Driven Decision Making: As a prominent feature in healthcare technology trends, it equips healthcare professionals with concrete data to base their decisions on, reducing reliance on guesswork and potentially decreasing the likelihood of medical errors.
Reduced Hospital Readmissions: Predictive analytics can identify patients at high risk of readmission. Healthcare professionals can provide targeted care post-discharge using this information, reducing patients’ chances to return to the hospital and improving long-term health outcomes.
Top 10 Predictive Analytics Applications in Healthcare
Predictive analytics in healthcare, a vital component of information technology in healthcare, is reshaping how healthcare organizations in the USA operate and care for patients. How? Let’s look into the applications of predictive analytics in healthcare to understand it.
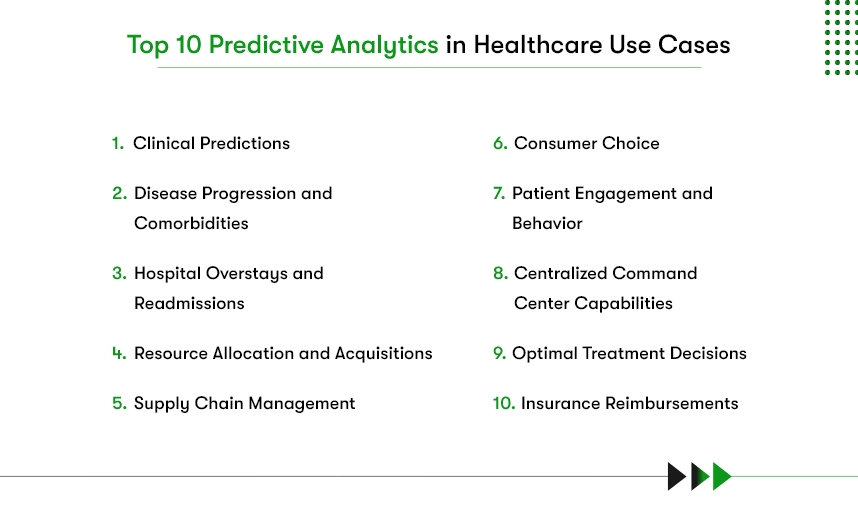
1) Clinical Predictions
Healthcare organizations utilize predictive analytics to assess the likelihood of patients developing conditions like cardiac problems, diabetes, stroke, or COPD. By integrating national, EHR, biometric, and claims data, models are created to predict disease likelihood on individual and community levels. By predicting developing conditions using predictive analytics, health insurance companies and healthcare providers can intervene early and improve health outcomes.
2) Disease Progression and Comorbidities
Predictive analytics is instrumental in identifying patients whose conditions might worsen. For example, it can predict which diabetes patients are at risk of developing renal disease. This early identification allows for early interventions that can drastically enhance patient outcomes, particularly in diseases like sepsis.
3) Hospital Overstays and Readmissions
By analyzing patient, clinical, and departmental data, predictive analytics can identify in-patients likely to exceed their expected length of stay. With this prediction, your healthcare facility can adjust protocols, ensuring care efficiency. It also identifies patients at high risk of hospital readmission, enabling clinicians to adjust post-hospitalization treatment plans. Thereby saving costs and improving patient outcomes.
4) Resource Allocation and Acquisitions
Predictive analytics also identifies patterns in resource allocation and predicts future needs. Hence, you can efficiently plan and acquire resources like CT scanners based on anticipated needs for effective usage.
5) Supply Chain Management
Managing the hospital supply chain has been challenging, and many still cling to the “the more is better” mindset. Consequences? Higher cost of mass acquisition and maintenance as well as waste of expired products. Though just in time is an option, it requires more workforce to execute.
However, you can use predictive analytics to forecast demand by leveraging historical and real-time data. For example, you can create a predictive analytics model that analyzes the data acquired from systems, including Electronic Healthcare Records. This model will predict the cases likely to emerge and the supplies required to treat those cases.
6) Patient Engagement and Behavior
Predictive Analytics helps healthcare entities understand and engage patients individually and as demographic groups. For instance, it can predict which patients will likely miss appointments or adhere to medication regimens, enabling more effective patient advocacy and healthcare messaging.
7) Consumer Choice
Healthcare providers can also use predictive analytics to improve patient satisfaction. Assessing clinician data to match suitable providers, predictive analytics can help patients select the healthcare facility based on specific needs.
For example, an elder health app solution equipped with a predictive analytics model can identify at-risk patients and manage health proactively, preventing hospital readmissions.
8) Optimal Treatment Decisions
Predictive analytics in optimal treatment decisions refers to using data analysis techniques to forecast the most effective treatment options for individual patients. It involves examining large sets of health data, including a patient’s genetic information, to identify patterns and predict outcomes.
For example, predictive analytics can find the best treatment for conditions like cancer for each patient using genetic data. It examines the patient’s unique genetic makeup and the characteristics of their cancer, allowing doctors to choose the most effective treatment quickly.
9) Insurance Reimbursements
In addition to core healthcare, predictive analytics can also help facilities manage their administrative and finance areas. For example, predictive analytics can analyze past claim data for insurance reimbursements to detect patterns that lead to denials or reduced payments.
Furthermore, armed with this knowledge, healthcare providers can optimize financial performance in billing and administrative areas, analyzing documentation for insurance claims and identifying potential issues.
10) Centralized Command Center Capabilities
Through healthcare app development, health IT vendors are integrating various predictive analytics applications and creating centralized command center capabilities. Such systems can predict and manage multiple aspects of hospital operations, combining various data sources into one place. For example, predicting the availability of ICU beds, the need for in-patient beds, or forecasting future requirements, Centralized command centers can help hospitals efficiently allocate resources.
With this advanced solution, healthcare facilities can better prepare to meet patient needs, improving patient care and experiences. It’s like having an advanced control tower that oversees and optimizes the entire hospital’s operations.
What are predictive analytics in healthcare examples?
Before going for Healthcare IT consulting to strategize your technology investments, you should know how existing leaders leverage predictive analytics.
Health Catalyst
Health Catalyst specializes in data and analytics technology, providing a foundation for healthcare systems in predictive analytics. Basically, they help healthcare professionals forecast clinical, operational, and financial needs and make data-driven decisions about them.
Health Catalyst collects data from various sources using the Data Operating System (DOS™), which is then aggregated into insights that support predictive models. For example, ChristianaCare used the Health Catalyst DOS™ platform to identify patients with COVID-19 who were at risk of hospitalization.
As a result, they achieved $1.8M in cost savings by avoiding 61 hospital admissions and seven intensive care unit admissions.
McKesson Corporation
McKesson Corporation is a leading healthcare supply chain management solutions provider. Using predictive analytics to analyze patient data and provide actionable insights, they help biopharma, pharmacies, care providers, and more.
Their approach includes refining drug procurement patterns and rendering formulary decisions to optimize drug profitability and accessibility.
Epic System
Epic System is a leading software company in the healthcare industry, known for its electronic health records system.
Partnering with a healthcare AI company, Pieces Epic provides predictive analytics tools in its marketplace. These tools offer physician-driven insights for early interventions and streamline the management of various cancers.
The integration of these tools in Epic’s EHRs assists clinicians in ordering and reviewing tests like the clonoSEQ Assay for monitoring minimal residual disease, enhancing cancer treatment and management
3 things worth your attention at the consideration stage of Predictive Analytics in Healthcare
Predictive Analytics in healthcare has made healthcare professionals curious to explore the possibilities the technology reserves. No matter how advanced technology is, it will still require subtle attention to things that do more harm than benefit if they go wrong.
So, if you’re looking forward to applying Predictive Analytics to your healthcare organization or startup, add the below consideration to your plan.
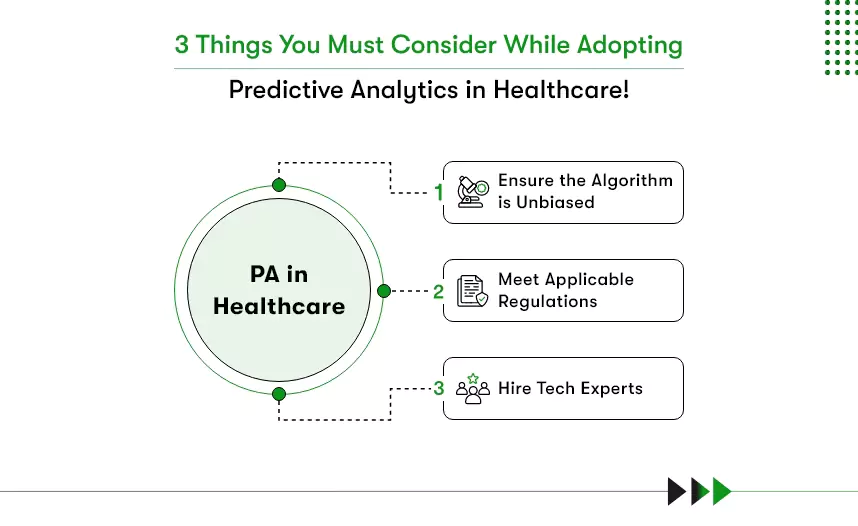
Algorithm Bias:
Think of algorithm bias like a medical test. If it’s inaccurate for everyone, it could mean some patients get misdiagnosed or receive inappropriate treatments. Ignoring bias could lead to unequal patient care, with certain groups getting left behind.
What should you do? Regularly check the “accuracy” of your algorithms, involve a diverse team in creating them, and use techniques that ensure fair results for everyone.
Regulations:
Just like following medical guidelines is crucial, sticking to healthcare regulations safeguards patient privacy and keeps your practice on the right side of the law. Overlooking regulations is like neglecting a patient’s medical history—some consequences are not good.
What should you do? Stay updated on the rules, put strong data protection measures in place, and do regular “compliance check-ups.”
Expertise:
Imagine using a new medical device without proper training—it’s risky. Without expertise in both data and healthcare, predictive analytics is like a tool in the wrong hands. It’s like treating patients with outdated methods. Results could be off, and decisions might not be in the patient’s best interest.
What should you do? Hire experienced developers who are predictive analytics specialists and have worked on healthcare technology.
Want to redefine healthcare services with Predictive Analytics?
According to HealthTech Magazine, an average healthcare facility generates roughly 50 petabytes of data every year through medical devices, genetic tests, EHR, etc. The amount of healthcare data is increasing at a rate of 47% per year, says the same study.
A smart healthcare professional or healthcare startup would know that this data is a gold mine. Leveraging technologies like NLP and Predictive Analytics, you can not only come up with better healthcare solutions but also provide preventive care.
Now, that can be groundbreaking! Don’t you think? What’s in it for you, you may ask? So, MarkeDigits reported,
The healthcare predictive analytics market, valued at $12.1 billion in 2022, is projected to reach $81.4 billion by 2030.
The market is lucrative, and giant technology and healthcare players like IBM have already started experimenting, aiming for a big breakthrough. What about you?








 Contact Information
Contact Information